What are Change Management Models in Healthcare?
In healthcare, change management models are conceptual frameworks that guide care organizations as they undergo significant transformation using tools, products, or services.
These frameworks ensure that changes are strategically and sustainably implemented as they affect the most granular aspects of clinical workflows. Systemic change will bring about differences in feedback, and the time to reconvene and align might cause disruption in care delivery. This highlights the use of various frameworks and theories to guide healthcare groups and direct teams to adopt innovative ways of performing daily tasks.
In this article, we’ll talk about change management models that apply to care organizations across varied focuses and specialties. We’ll also see how you can implement human-centered changes, from theory to practice.
The Importance of Change Management Theories in Healthcare
The rapid development of innovation in healthcare technology drives the increasing prioritization of healthcare quality. Subsequently, this impacts how change management models drive healthcare organizations to handle transitions in the least disruptive ways.
While change can naturally be grueling for care systems, research shows that projects are successful when led by clinicians, as they stay engaged with the momentum that drives change activities. Conversely, the change may face greater difficulties if the benefits are not clearly defined for clinicians, patients, and staff from the beginning.
As a system, healthcare is complex; hence, there is a constant need to adapt to more innovative ways of working. This underpins why understanding established concepts of site-wide transition is essential, especially for directors and clinicians who typically are the motivators, the agents of change in healthcare.
Change Management Models Comparison
In this section, we compare the change management methodologies found to be the most commonly used in healthcare as they are comprehensively well-suited in driving sustained changes. To be more cohesive, we’ll also tackle it in the context of clinical practice.
The table below compares the most relevant change management models in healthcare.
| Change Management Model Characteristic | ADKAR Change Model | Kotter’s Theory of Change | McKinsey 7S Model | Lewin’s Change Management Model |
|---|---|---|---|---|
| Primary Unit of Change | Individual clinicians and staff members | Organisational groups led by change leaders | Entire organisation | Teams as a collective |
| Change Progression Style | Incremental and capability-based | Sequential and momentum-driven | Diagnostic and alignment-focused | Stage-based (before, during, after change) |
| How Progress Is Tracked | Measurable checkpoints per individual | Reinforced through visible milestones | Assessed through consistency across elements | Stabilisation after refreezing |
| Speed of Adoption | Gradual, habit-forming | Accelerates through early wins | Varies based on organisational readiness | Moderate, paced by stages |
| Best Applied When | Introducing new tools or workflows requiring individual adoption | Driving large-scale initiatives that need sustained energy | Preparing for complex, system-wide change |
We have gleaned an overview of how these change management models are similar and different from one another. Understanding how these models differ is a step towards building an approach that promotes buy-in among stakeholders.
At the Dudley Group NHS Foundation Trust, clinicians and leaders put Heidi to the test in one of the most comprehensive NHS evaluations of ambient AI to date. Over three months across Same Day Emergency Care and Rheumatology, Heidi produced significant clinical outcomes, such as reducing documentation time by 71% and returning more than 2,600 billable hours per year.
A consultant happily shared, "I had a really overbooked HOT clinic with complicated patients...Heidi saved me 5-10 minutes per patient to dictate the letter and also the brain power to think about the letter content.... it made a horrendous clinic much more manageable."
With Heidi in practice, more than 90% of patients reported feeling more listened to as consultations became more natural and personal. Clinicians also described Heidi as “the most helpful tool ever offered,” citing lower fatigue, sharper focus, and greater satisfaction at the end of demanding shifts.
The Dudley results show what happens when technology strengthens clinical presence rather than competes with it. As shared by a nurse, "I was able to see patients back to back rather than spending time in between documenting.”
The next section will explore further the different types of change management models with real-world context. The theories abovementioned will be further broken down below through clinical illustrations.
Types of Change Management Models with Examples
Change management models build confidence among care teams and clinicians to support them in delivering care with minimal disruption and streamlined collaboration.
As the industry embraces digital transformation, leaders face the challenge of aligning technology with the human side of care. Heidi is on board with this evolution by turning change management principles into actionable workflows.
Let’s take a closer look at how these frameworks guide transformation and how Heidi helps care teams put them into practice.
1. ADKAR Change Management Model
The ADKAR theory of change management works well for clinicians adopting new technology, or in this context, AI tools. This is due to its concept that change in behavior is an incremental skill acquisition in itself. The title of the theory is an acronym that pertains to outcomes that change agents aim to achieve:
- Awareness
- Desire
- Knowledge
- Ability
- Reinforcement
This approach is rooted in habit-forming and minimizing disruption of workflows. In healthcare, Heidi helps address resistance as its value proposition aligns with the principles of this model.
For instance, success in change implementation can look like adoption through a very simple onboarding, not requiring clinicians to click more buttons or profound technical skill.
2. Kotter’s 8-Step Change Management Model
John Kotter’s eight-step framework focuses on components like leadership, urgency, and momentum, around which a successful change implementation is built. In this model, success is dependent on care leaders’ ability to communicate and efforts to align initiatives for quality improvement.
Mainly ideal for large organizations, this approach highlights vision-building as a strategy to inspire and unify local change agents like clinicians.
To manage change, here are the eight steps from this model:
- Create a sense of urgency
- Build a guiding coalition
- Form a strategic vision
- Enlist a volunteer army
- Enable action; Remove barriers
- Generate short-term wins
- Sustain acceleration
- Institute change
In essence, this model emphasizes the role of change agents as crucial in minimizing resistance. In healthcare, this framework ensures changes are not only implemented but also sustained through collaboration.
With Heidi, teams can gain visible early wins in daily practice. Specialists and GPs can save up to 500 hours weekly on documentation, and experience reduced levels of burnout.
3. McKinsey’s 7S Change Management Framework
McKinsey’s 7-S of change management is built around seven interconnected elements as follows:
- Strategy
- Structure
- Systems
- Shared Values
- Skills
- Style
- Staff
This model does not provide a step-by-step process, but it rather allows healthcare teams to focus on the seven factors to facilitate change. It is effective for assessing readiness across hospital systems that are complex in nature, before major overhauls of digital processes.
Ultimately, any change management model is only as strong as the people empowered to use it. Heidi bridges that gap. It helps identify structural barriers that can stall momentum if you want to scale up.
4. Lewin’s 3-Stage Change Management Theory
Kurt Lewin’s change structure highlights three stages that align with improvement cycles in healthcare.
- Unfreeze
- Change
- Refreeze
The simplest of the popular theories of change, this approach focuses on the collective mindset and behavioral shift instead of organizational design. Habit formation is the key goal, and this is common for companies that introduce policy shifts or procedural protocols.
Successful change relies on trust and participation from care professionals. Heidi complements this by giving clinicians intuitive tools that allow change to feel natural.
Heidi is more than an AI medical scribe. Our AI care partner has been intentionally redesigned to be better, facilitating the "unfreeze" of complex, outdated documentation workflows and their "refreeze" as automated clinical processes. This transformation is effective for both small teams and large enterprise-level groups.
Relevant studies have found that the type of change management approach implemented matters less during this monumental period. The key is implementing change while maintaining adaptability and flexibility, so that change agents like clinicians can empower others and improve support. When this flexibility is present, success rates are highly likely, no matter the change management theory employed.
How can clinicians like you participate in driving the successful implementation of change?
Turn Change Into Progress with Heidi By Your Side
Change succeeds when people and technology move together. There is no single “right” approach to successfully implement major transformation within care teams. Change management theories can be integrated when put into practice, and you can maximize your resources with Heidi by your side.
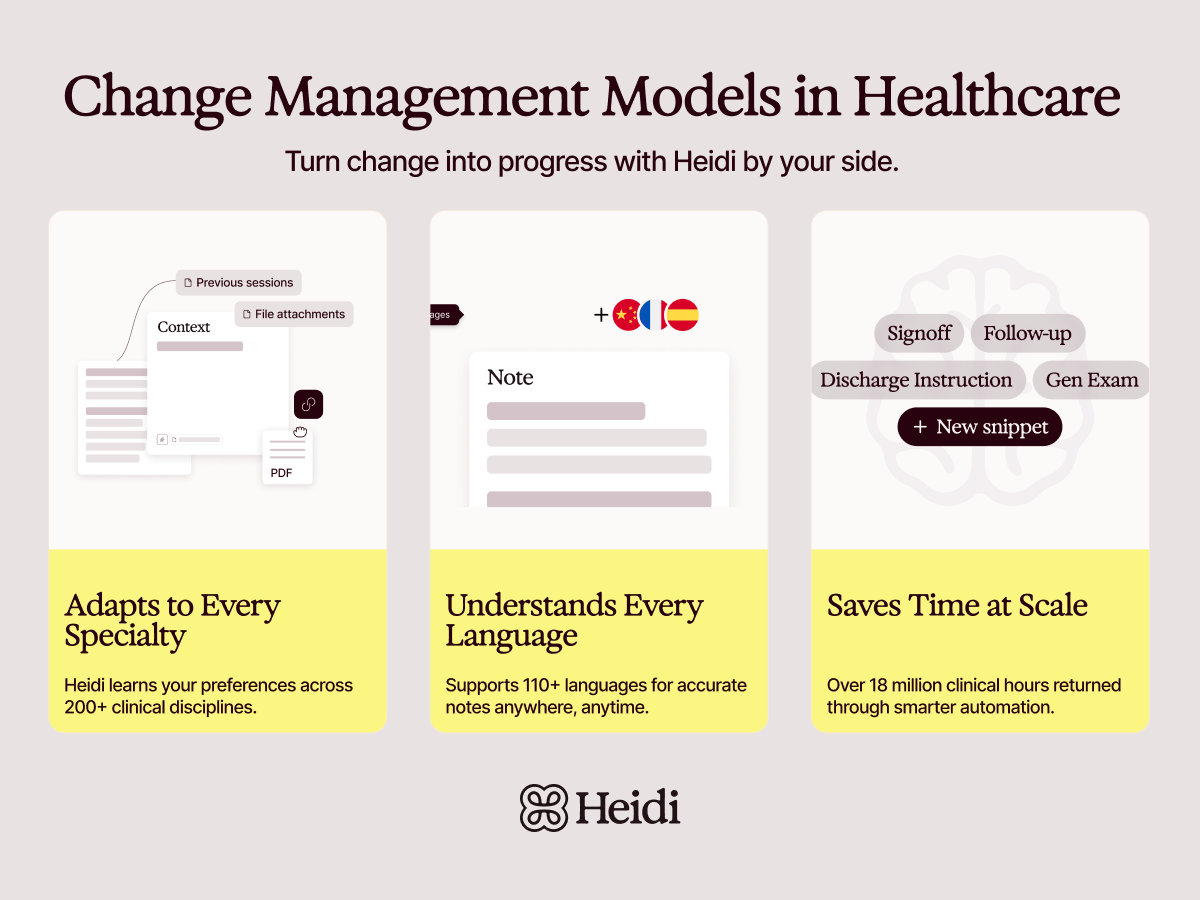
All specialties considered in practice, you will never have to worry about delays and work disruption, knowing that Heidi:
- Adapts to over 200+ specialties - Over time, Heidi learns and adapts to your personal preferences and terminology when using templates for tailored documentation.
- Supports over 110 languages - Heidi’s AI can work in remote areas, noisy environments, or low-connectivity settings. Its context-awareness processes transcription in real-time, yielding notes that are highly accurate.
Frequently Asked Questions About Change Management Models in Healthcare
Context matters in assessing the most effective change management model in healthcare. For instance, care teams can employ the ADKAR model in driving individual clinical adoption, while Kotter’s 8-step theory is stronger for transformations in hospitals.
